General Considerations
Indications:
- Diagnosis of meningitis, subarachnoid hemorrhage, carcinomatosis, multiple sclerosis, etc.
- Measurement of CSF pressure (e.g., normal pressure hydrocephalus).
- Delivery of medications (e.g., spinal anesthesia or intrathecal chemotherapy).
- Relief of increased intracranial pressure in rare situations (e.g., cryptococcal meningitis).
Contraindications:
- Absolute:
- Infection over or near puncture site.
- Relative:
- Increased intracranial pressure (with Neurology input); if suspected (e.g., papilledema, headache), evaluate with head CT.
- Coagulopathy or DIC (should reverse coagulopathy if INR >1.5 and/or platelets <50K).
- Prior lumbar fusions/surgeries (may need paraspinal approach or image-guidance).
When Should I Get a CT Prior to LP?
If your patient has any of the following criteria, you should get a non-contrast head CT prior to LP to minimize the risk of brainstem herniation (97% negative predictive value if none of the following are present in patients with suspected meningitis):
- Age >60 years.
- Immunocompromised state.
- History of CNS lesion (mass lesion, stroke, and/or focal CNS infection).
- Seizure in the week prior to presentation.
- Neurologic findings (altered mental status, inability to answer two questions or follow two commands correctly, and/or any focal neurologic deficits).
Technique
Preparation:
- Obtain informed consent.
- Review procedure with your supervisor and watch the NEJM “Lumbar Puncture” video.
- Gather supplies: LP kit (has a standard 20g Quincke needle), additional atraumatic needle (called Sprotte or Pajunk 20g or 22g) if desired, 10mL 1% lidocaine, chlorhexidine, labels for sample bottles, black top tube(s) (for cytology or other infectious studies), 2 sets of sterile gloves, 2 face masks with shields, chuck, wastebasket, additional helpers to position patient.
- Hold enoxaparin for 12 hours for prophylactic and 24 hours for therapeutic dosing. Heparin prophylaxis is thought to be relatively safe, although ideally avoid close to LP.
- If multiple specialized tests are needed, know in advance the approximate CSF amount needed for each vial, which will guide how many extra tubes are needed.
- At UCSF, you can look up any test and the required fluid amount in the on-line lab manual.
Procedural steps:
- Perform Time-Out. Complete and have an assistant co-sign the pre-procedure checklist.
- Positioning is key. Place patient on side with shoulders and pelvis perpendicular to the bed, hips flexed as much as able, pillow between legs for comfort, and lumbar region parallel to edge of bed (or alternatively sitting at the edge of the bed leaning over a table).
- Identify the top of each posterior iliac crest. The line that connects these typically crosses the L4 spinous process. L3-L4, L4-L5, and L5-S1 are safe spaces to attempt a bedside LP. Mark at least two different spaces.
- Use sterile technique to prep and drape site. Ensure chlorhexidine is completely dry prior to inserting needle due to risk of aseptic meningitis.
- Use a 25g or smaller needle for your initial wheal and subcutaneous anesthesia. Change to a 22g needle and while holding the needle perpendicular to the patient, infuse lidocaine and advance to the level of the vertebrae or until the needle is hubbed.
- Insert spinal needle (bevel pointing up to ceiling if lying and laterally if sitting up) into the interspace and advance slowly with slight cephalad angle, aiming towards the umbilicus. Periodically stop and remove stylet fully to check for CSF but replace stylet prior to any motion of the needle.
- Once subarachnoid space reached and CSF is draining, attach manometer and measure pressure (controversial if leg position affects opening pressure, but not recommended to change positioning due to patient safety).
- Drain CSF into tubes 1-4 using only the minimal amount needed for all desired studies. The less CSF removed, the less chance for headache.
- For standard tests, 2ml are needed per tube.
- If sending for AFB, ideally collect 15mL and for cytology ideally 10mL.
- Re-insert stylet, remove needle, and apply dressing.
- If having difficulty, can withdraw and go in different intervertebral space. Ensure optimal positioning. If difficulty persists, consider neuroradiology consult for a CT-guided LP.
Complications
- Headache, back pain, infection, hemorrhage, brainstem herniation, paralysis.
Post-LP headache:
- Most common side effect (~30% of patients) from the procedure thought to be from persistent CSF leakage.
- Practices supported by evidence: less CSF removed is better, atraumatic needle is better, smaller needle may be better (usually 22g), needle bevel orientation should be parallel to spine, stylet should be re-inserted when removing the needle, and patient should be mobilized when ready.
Diagnostic Studies
Check your hospital for specific guidelines on which studies are performed on individual tubes and what the normal reference ranges are. Typically check cell count/differential, glucose, total protein, gram stain, and culture. You can add other chemistries and microbiologic/cytologic tests as clinically indicated.
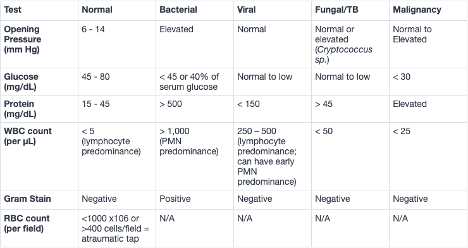
*Normal opening pressure in cmH2O is <20.
Tip: to correct for a traumatic tap, subtract one WBC for every 500-1500 RBC.
Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med 2001;345(24):1727-33.
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA 2006;296(16):2012-22.
Williams J, Lye DC, Umapathi T. Diagnostic lumbar puncture: minimizing complications. Intern Med J. 2008;38(7):587-91.