Berlin Definition of ARDS
|
Timing |
Within 1 week of known clinical insult or new/worsening respiratory symptoms |
|
Chest imaging |
Bilateral opacities that are not explained by effusions, lobar/lung collapse or nodules |
|
Origin of edema |
Not fully explained by cardiac failure or volume overload |
|
Oxygenation |
Mild: PaO2/FiO2 = 200-300mmHg with PEEP or CPAP ≥5cmH2O Moderate: PaO2/FiO2 = 100-200 with PEEP 5cmH2O Severe: PaO2/FiO2 ≤100mmHg with PEEP 5cmH20 |
Pathophysiology
Inflammation in the lungs from a direct (e.g., pneumonia) or indirect (e.g., pancreatitis) cause that results in damage to the capillary endothelium and alveolar epithelium resulting in accumulation of proteinaceous fluid in the air spaces and alveolar collapse. As a result:
- Gas diffusion is impaired -> hypoxemic and, when severe, hypercarbic respiratory failure.
- Lungs are stiff from poor aeration (reduced compliance) and at risk of barotrauma.
ARDSNet Protocol
Tidal volume goal:
- The tidal volume (VT) goal is LOW at 4-8cc/kg predicted body weight (start at 6cc/kg and adjust if oxygenation, plateau pressures, or ventilation/pH not at goal).
- Predicted body weight (PBW): for females, PBW = 45.5 + 2.3 (height in inches - 60); for males, PBW = 50 + 2.3 (height in inches - 60).
- The plateau pressure (PPL) goal is ≤30cmH20.
- Adjust VT (4-8cc/kg) to achieve PPL 25-30.
- If PPL >30cmH2O, decrease VT in 1cc/kg increments.
- If PPL <25cmH2O and VT<6cc/kg, increase VT by 1cc/kg until PPL >25cmH2O or VT= 6cc/kg.
- If PPL <30 and breath-stacking or dyssynchrony, increase VT in 1cc/kg increments to 7 or 8cc/kg if PPL remains <30cmH2O.
Oxygenation goal:
- PaO2 of 55-80mmHg or O2 sat of 88-95%.
- There are two grids: “low” PEEP (e.g. ARMA) and “high” PEEP (e.g. ALVEOLI, LOV, Express trials).
pH goal: permissive hypercapnia.
- pH = 7.30–7.45.
- Low tidal volume ventilation often impairs ventilation which is usually well-tolerated and termed permissive hypercapnea. It is very rare to need to increase tidal volume to manage.
- Adjust respiratory rate (max 35) and consider NaHCO3 or THAM to keep pH at goal.
I:E ratio:
- The goal I:E ratio is 1:1–1:3. Adjust flow rate and inspiratory flow to achieve this goal.
Conservative Fluid Management
- The FACTT RCT showed a conservative fluid strategy with diuresis (goal CVP <4, PCWP <8) resulted in better oxygenation, fewer ventilator-days, and shorter ICU stay without a difference in non-pulmonary organ failure compared to a liberal fluid management strategy.
- Excluded patients with hypotension, pressors, oliguric renal failure, or HD.
Refractory Hypoxemia
ARDSNet protocol requiring FiO2 of 0.8 or higher, especially if at 1.0 – see Critical Care: Advanced Strategies in ARDS for details, in brief:
- Paralyze the patient to decrease oxygen consumption and improve synchrony.
- Place the patient in the prone position to improve ventilation-perfusion matching.
- Try a recruitment maneuver to recruit collapsed alveoli.
- Can consider low-dose inhaled nitric oxide to improve oxygenation but not mortality.
- If all else fails, try a different ventilatory mode (APRV, PCV) or consider ECMO.
ARDS Studies and Protocols
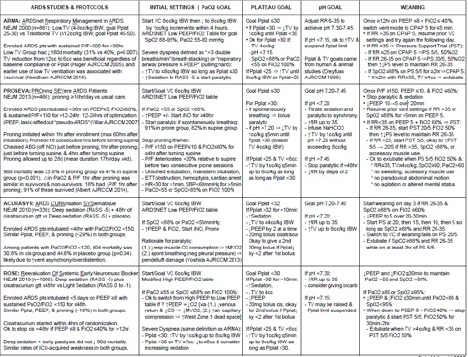
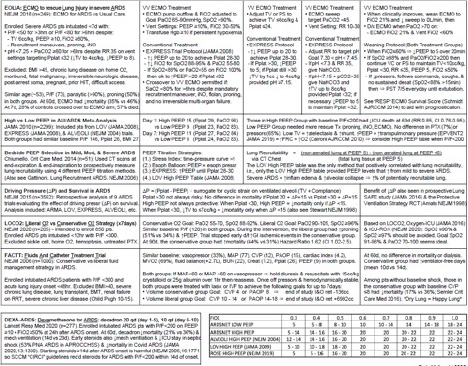
ARDSnet Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000;342:1301-1308.
Barrot L, Asfar P, Mauny F, et al.; LOCO2 Investigators and REVA Research Network. Liberal or Conservative Oxygen Therapy for Acute Respiratory Distress Syndrome. N Engl J Med. 2020 Mar 12;382(11):999-1008. doi: 10.1056/NEJMoa1916431. PMID: 32160661.
Combes A, Hajage D, Capellier G, et al.; EOLIA Trial Group, REVA, and ECMONet. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2018 May 24;378(21):1965-1975. doi: 10.1056/NEJMoa1800385. PMID: 29791822.
Fan E, Del Sorbo L, Goligher EC, et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome [published correction appears in Am J Respir Crit Care Med. 2017 Jun 1;195(11):1540]. Am J Respir Crit Care Med. 2017;195(9):1253-1263. doi:10.1164/rccm.201703-0548ST
Guérin C, Reignier J, Richard JC, et al.; PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013 Jun 6;368(23):2159-68. doi: 10.1056/NEJMoa1214103. Epub 2013 May 20. PMID: 23688302.
Malhotra A. Low tidal volume ventilation in the acute respiratory distress syndrome. N Engl J Med 2007;357:1113-1120.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006 Jun 15;354(24):2564-75. doi: 10.1056/NEJMoa062200. Epub 2006 May 21. PMID: 16714767.
National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Moss M, Huang DT, Brower RG, et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. N Engl J Med. 2019 May 23;380(21):1997-2008. doi: 10.1056/NEJMoa1901686. Epub 2019 May 19. PMID: 31112383; PMCID: PMC6741345.
Papazian L, Forel JM, Gacouin A, et al.; ACURASYS Study Investigators. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010 Sep 16;363(12):1107-16. doi: 10.1056/NEJMoa1005372. PMID: 20843245.
The ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA. 2012:307(23):2526-33.
Villar J, Ferrando C, Martínez D, et al.; dexamethasone in ARDS network. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020 Mar;8(3):267-276. doi: 10.1016/S2213-2600(19)30417-5. Epub 2020 Feb 7. PMID: 32043986.