Modes of Ventilation
Volume Controlled:
- AC (Assist Control):
- Set the rate, tidal volume, FiO2, PEEP. The amount of inspiratory pressure will vary based on the compliance of the patient’s lungs.
- Example: on AC with rate of 12 and tidal volume of 700cc, the ventilator will deliver 12 breaths per minute, each with a volume of 700cc. If the patient initiates a breath independently, the ventilator will deliver a volume of 700cc for that breath.
- Tachypnea in this mode may therefore cause respiratory alkalosis. Good mode for patients who require a constant tidal volume and maximal ventilatory support.
- SIMV (Synchronized Intermittent Mandatory Ventilation):
- Set the rate, tidal volume, FiO2, PEEP; also set pressure support for non-supported breaths. Again, inspiratory pressure depends on pulmonary compliance.
- Example: on SIMV with a rate of 12 and tidal volume of 700cc, the ventilator will deliver 12 breaths/min, each with volume of 700cc. If the patient initiates an additional breath independently, the ventilator will provide pressure support (at a level you set), but does not deliver a preset volume.
- This mode therefore may improve patient synchrony with the vent and decrease the risk of respiratory alkalosis, but may require more respiratory muscle work than AC.
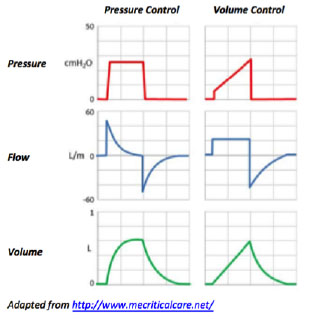
Pressure Controlled:
- PC (Pressure Control):
- Set the rate, inspiratory pressure, FiO2, PEEP. The tidal volume will vary based on pulmonary compliance.
- Example: on PCV with a rate of 12 and inspiratory pressure of 25, the ventilator will deliver 12 breaths per minute, each with an inspiratory pressure of 25cmH2O.
- Peak pressures are constant (peak = PEEP + inspiratory pressure).
- Risks include hypoventilation as tidal volume may change dramatically with a change in respiratory compliance. This mode may improve patient synchrony with the ventilator, but should be used with caution and adequate blood gas monitoring.
Other:
- PS (Pressure Support):
- Set the inspiratory pressure, FiO2, PEEP. Patient will determine rate and tidal volume.
- Example: at pressure support 15/5, the ventilator has a constant 5cmH2O of PEEP, and when the patient initiates a breath, the ventilator supports the breath with 15cm H2O.
- This is a flow-limited mode of ventilation and the ventilator will terminate the pressure when the patient’s inspiratory flow falls to a set percentage of peak flow (usually 25%). This is how the ventilator detects that the breath is complete.
- Risks include hypoventilation or apnea because the patient must trigger the ventilator and there is no mandatory minute ventilation. This mode of ventilation is best used in patients who are being weaned from the ventilator. Consider using in conjunction with order set that implements volume-limited modes overnight to rest patients.
- BiPAP: similar to pressure support when intubated, for noninvasive use please see section Noninvasive Positive Pressure Ventilation (NIPPV) BiPAP or CPAP.
- CPAP (Continuous Positive Airway Pressure):
- The ventilator maintains a constant level of positive pressure during entire respiratory cycle.
- This is equivalent to using the PS mode with the PEEP set to the desired CPAP level and the pressure support set to zero. It is best suited for patients with sleep-related breathing disorders such as OSA or OHS, or during a spontaneous breathing trial (SBT). For noninvasive use please see section Noninvasive Positive Pressure Ventilation (NIPPV) BiPAP or CPAP.
Initial Ventilator Settings
- Mode: usually AC-VC.
- Rate = 12 (lower rates may be needed in patients with COPD/asthma to avoid auto-PEEP and higher rates may be needed in patients with metabolic acidosis and sepsis). In addition to adjusting rate, consider decreasing inspiration to expiration (I/E) ratio (e.g. 1:4) in patients with obstructive airway disease.
| auto-PEEP refers to the phenomenon in which a breath is delivered by the ventilator before a patient is able to fully expire – “breath stacking” – thus resulting in an ever increasing volume of air within the lungs and increased intrathoracic pressure that ultimately may cause hypotension due to impaired venous return. |
- Tidal volume (VT) = 8cc/kg predicted body weight (lower in ARDS, see section Acute Respiratory Distress Syndrome). There is growing evidence that lung-protective ventilation is beneficial in non-ARDS patients (e.g. from anesthesia literature), so lower tidal volumes should be utilized whenever possible. Predicted body weight is calculated from gender and height. If you don’t know this already, 400-500cc is a reasonable starting place for most patients.
- FiO2 = 1. Wean down rapidly as tolerated to ≤70% to avoid oxygen toxicity.
- PEEP (positive end-expiratory pressure) = 5-20. Start at 5-8, adjust accordingly and use cautiously in COPD/asthma due to risk of auto-PEEP.
- Pressure support usually set at 5-10 for SIMV.
Adjusting Ventilator Settings: the very basics
- Oxygenation: for low pO2, increase FiO2 or PEEP (increasing PEEP may recruit more alveoli).
- Ventilation: for high pCO2, increase the tidal volume or rate (also try suction, bronchodilators).
Weaning Parameters
In absence of contraindications, standard of care includes daily weaning trials to facilitate earlier extubation. The following requirements should be met prior to considering extubation:
- Improvement of the initial indication for mechanical ventilation (e.g. pneumonia).
- Hemodynamic stability (stable low-dose vasopressor infusion often okay).
- The patient must be neurologically stable and able to protect the airway (wean sedation).
- Adequate oxygenation: pO2 >60 on ≤40% FiO2 and PEEP ≤8.
- Airway patency: check cuff leak (respiratory care or ICU physician can help with this).
Weaning Strategies
- PS recommended. CPAP and T-piece can be considered alternatively.
- When ventilator support has been lowered to a pre-specified level (institution-specific, e.g. PEEP <8cmH2O, FiO2 <0.5), daily spontaneous breathing trials (SBT) should take place.
- Daily sedation interruption paired with daily spontaneous breathing trial (SBT) are standard of care as they increase ventilator-free days and decrease ICU and hospital LOS.
- Guidelines recommend initial SBT be performed at low-level pressure support (5-8cmH2O). Alternatives include a T-piece, or CPAP. Low level PS is preferred due to higher SBT and extubation success rates. Consider SBT on PS at higher settings (if clinically appropriate) even when patients are not near extubation.
- Practice guideline: perform SBT with any method for 30 minutes and check a rapid shallow breathing index (Tobin index), work of breathing, and hemodynamics. Consider extended SBT up to 2 hours for patients with prolonged intubation (>10 days) or neuromuscular weakness.
Tobin index = Respiratory rate / Tidal volume (L) < 105 predicts weaning success - With all methods, assess ABG, RR, TV, HR, BP, work of breathing, and mental status to determine when extubation is appropriate.
Criteria for Extubation
- Reversal or improvement of the underlying indication for intubation.
- Hemodynamic stability (stable low-dose vasopressor infusion almost always okay).
- Adequate oxygenation on minimal vent settings and spontaneous respiration (pO2 >60 on ≤40% FiO2 and PEEP ≤8).
- Rapid shallow breathing index (Tobin index) ≤ 105.
- Intact mental status with airway protection (follows commands, adequate cough, gag, and minimal secretions).
- Airway patency: check cuff leak (RT or ICU MD can assist with this).
- Minimal secretions/suctioning requirements.
Post-extubation Oxygenation Strategies
- Low risk of post-extubation failure: standard is to extubate to nasal cannula, however there is growing evidence that extubation to high flow nasal cannula (HFNC) may increase success rate. Worth considering for patients with ongoing mild respiratory failure or persistent secretions.
- High risk of post-extubation failure (in general patients who are older, obese, have significant chronic lung or heart disease, have ongoing high secretions, or intubated for pneumonia):
- Extubation to nasal cannula is always an option.
- BiPAP (or CPAP): consider for patients with predisposition to hypercarbia such as COPD, OSA, severe obesity, neuromuscular weakness, severe kyphosis, or if using non-invasive ventilation as a weaning strategy.
- HFNC is more comfortable and better tolerated than BiPAP and has been shown to reduce re-intubation for all patients, including those prone to hypercapnia (can consider BiPAP first line and transition to HFNC if not well tolerated).
- Planned use of these strategies is supported by evidence while rescue use (i.e. after respiratory distress develops) carries a risk of harm from delayed re-intubation and should be used cautiously and with frequent re-assessment.
Failure to Wean
|
F |
Fluid overload → diurese if indicated |
|
A |
Airway resistance → check endotracheal tube; is it obstructed or too small? |
|
I |
Infection → treat as indicated |
|
L |
Lying down causing V/Q mismatch → elevate head of bed |
|
T |
Thyroid, toxicity of drugs → check TFTs, check med list |
|
O |
Oxygen → increase FiO2 and/or the level of PEEP |
|
W |
Wheezing → treat with bronchodilators |
|
E |
Electrolytes, eating → correct K/Mg/PO4/Ca, provide adequate nutrition |
|
A |
Anti-inflammatory needed? → consider steroids in asthma/COPD or for failed cuff |
|
N |
Neuromuscular disease, neuro status compromised → myasthenia gravis, ALS, steroid/paralytic neuropathy, etc.; assure that patient is neurologically stable |
Patients with Prolonged Mechanical Ventilation
- Tracheostomy:
- Improves patient comfort and communication, reduces sedation requirements, facilitates ventilator weaning, and mobilization (PT!) while on the ventilator.
- Timing of tracheostomy remains controversial. A 2010 RCT comparing early (within 7 days) to late (after 2-3 weeks) demonstrated earlier tracheostomy had better weaning, earlier ICU discharge, and lower rates of VAP but no survival difference. In general, start thinking about tracheostomy after 1-2 weeks of mechanical ventilation.
- Early mobilization: in appropriate patients, initiate physical and occupational therapy within 1-2 days of intubation. Patients are assisted in sitting at edge of bed, standing, moving to a chair, and, in some cases, ambulating.
- Demonstrated benefits include decreased ICU and hospital LOS, improvements in strength and functional status, and decreased ICU delirium.
Caring Wisely: don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions --> no daily chest x-rays!
Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet. 2008 Jan 12;371(9607):126-34.
Hess DR. The role of noninvasive ventilation in the ventilator discontinuation process. Respir Care. 2012;57(10):1619-1625.
Hodgson CL, Berney S, Harrold M, et al. Clinical review: early patient mobilization in the ICU. Crit Care. 2013 Feb 28;17(1):207.
Ouellette DR, Patel S, Girard TD, et al. Liberation From Mechanical Ventilation in Critically Ill Adults: An Official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline: Inspiratory Pressure Augmentation During Spontaneous Breathing Trials, Protocols Minimizing Sedation, and Noninvasive Ventilation Immediately After Extubation. Chest. 2017;151(1):166-180.
Terragni PP, Antonelli M, Fumagalli R, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA. 2010;303(15):1483.
Zhu, Y., Yin, H., Zhang, R. et al. High-flow nasal cannula oxygen therapy versus conventional oxygen therapy in patients after planned extubation: a systematic review and meta-analysis. Crit Care 23, 180 (2019).