Introduction
- Point of care ultrasound done at the bedside to aide in diagnosis or management and answer specific clinical questions. Caveats: not a quantitative analysis.
- Key acute uses: evaluation of volume status, cardiac tamponade, ventricular size and dysfunction, severe valvular dysfunction.
- Transducer has a notch on one side for orientation which corresponds to the orientation marker on the monitor, which is on the upper right of the image by convention.
- Gain: amplification of images. More gain = more white on the screen.
- Five point of care cardiac views (link) using the phase-array (cardiac) probe.
Parasternal Long Axis

- Uses: size and contractility of ventricles, morphology and function of mitral and aortic valves, ascending aorta, pericardial effusions.
- Position: left lateral border of sternum, 3rd-4th intercostal space, notch pointing to R shoulder (10 o’clock).
- Depth: 12-16cm for cardiac chambers, 20-24cm for pericardial or pleural effusions.
- Quality: septum and LV wall should be horizontal, LV apex should not be visualized, AV and MV should be seen and in center of screen, but TV should not be seen. If possible, place patient in left lateral decubitus for parasternal views.
- For LV function in this view you should look for LV wall thickening, good movement of the base of the heart, and the E point septal separation (distance of the anterior leaflet tip to the septum in diastole to assess LV function). A large E point septal separation suggests decreased LV function.
- For LV size – If the LV dimension in diastole is > 6cm in men or >5 cm in women the LV is dilated.
- If fluid is seen anterior to the descending aorta then it is a pericardial effusion, if posterior to the descending aorta it is a pleural effusion.
Parasternal Short Axis – Mid Ventricle

- Uses: size and contractility of ventricles, evaluate EF, wall motional abnormalities, pericardial effusion.
- Position: start from parasternal long axis, rotate 90 degrees clockwise (notch pointing to L shoulder) while keeping aortic valve centered on screen.
- Depth: 12-16cm.
- Quality: at papillary muscle level, LV should be round and in middle of the screen.
- If the septum is flattened and the RV is enlarged making the LV D-shaped during the cardiac cycle this can be from pressure overload (systolic only septal flattening), volume overload (diastolic only septal flattening) or both (systolic and diastolic flattening).
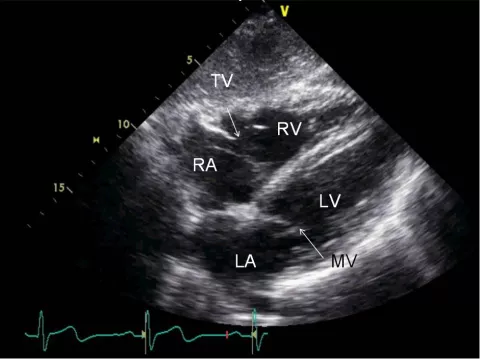
Apical Four-Chamber

- Uses: can assess chamber sizes, LV and RV function and for RV/RA diastolic collapse in tamponade.
- Position: apex of LV (apical impulse). Notch points at R shoulder (2 or 3 o’clock).
- Depth 14-18cm.
- Quality: LV apex close to probe and all four chambers seen and long axis of heart vertical, abduct patient’s left arm to improve window. If possible, place patient in left lateral decubitus for apical views.
- For RV function see how well the RV base to apex motion is using the tricuspid annulus to tell. RV size is normally 2/3 size of LV, if same size as or larger than the LV then this is abnormal. In tamponade you might see RV diastolic collapse and RA diastolic collapse.
Subcostal Four-Chamber
- Uses: assess cardiac chambers, pericardial effusion.
- Position: 2-3cm below the xyphoid, notch at 3 o’clock, press down and angle upwards the left shoulder. Overhand the transducer with the palm down to facilitate flattening of the probe.
- Depth: 16-24cm.
- Quality: patient with bent knees if possible, have patient take deep breath and hold
- Similar to the apical four-chamber but allows you to see the RV free wall a little better and any anterior pericardial effusions.
Subcostal Inferior Vena Cava

- Uses: assess volume status.
- Position: from the subcostal 4 chamber view, rotate transducer 90 deg counter-clockwise (notch towards head) while keeping the RA in view
- Quality: IVC merging with RA, measure IVC 2-3cm inferior from this junction.
- To tell it is the IVC you should see it 1) IVC emptying into the RA, 2) visualize the hepatic vein 3) be able to use color to show blood coming to the heart – blue flow.
- When evaluating collapsibility keep IVC in plane (probe can slide out of view with respiration).
- In spontaneously breathing patients:
|
IVC size (cm) |
Collapsibility during sniff |
Estimated RA pressure (mmHg) |
|---|---|---|
|
≤ 2.1 |
>50% |
0-5 |
|
>2.1 |
>50% |
5-10 |
|
>2.1 |
<50% |
10-20 |
References
Images courtesy of Atif Qasim MD from http://echocardiographer.org/TTE.html
Beraud AS, Burkett T. Introduction to transthoracic echocardiography, <http://viewer.zmags.com/publication/3c9e5062#/3c9e5062/1>
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocar- diography. Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 2010;23:685-713.